Recent Outbreaks of Anthrax In The West-African Sub-region
The earliest known description of anthrax is found in the Book of Genesis, in which the fifth plague is said to have killed Egyptian cattle.
Encyclopedia of Toxicology
The Federal Ministry of Agriculture & Rural Development in Nigeria has warned the public about Anthrax outbreaks in some nearby countries in West Africa, particularly in Northern Ghana, which borders Burkina Faso and Togo.
According to reports, the disease has already claimed some lives in areas of outbreaks, warranting the government to alert the public on steps to prevent the transmission of the disease.
People in contact with domesticated ruminants are at higher risk of contracting Anthrax from infected animals.
The government issued a public health warning advising people to avoid eating bush meat, cowhide (known as ‘ponmo’ locally), and smoked meat for the time being. These foods pose a serious risk until the situation is brought under control.
The ministry has assured the people that it’s doing all it can to bring the situation under control, including alerting responsible authorities, resuscitating a Standing Committee on the Control of Anthrax in the Ministry of Agriculture and Rural Development and collaborating with relevant institutions, like state directors of veterinary services nationwide.
This article takes an in-depth look at the disease, from the description, epidemiology, pathophysiology, medical treatment and diagnosis and more.
It’s intended for readers with medical or healthcare backgrounds.
As of writing, there has yet to be an official report from NCDC, CDC or WHO as regards the situation.
What Is Anthrax?
Anthrax is an infectious disease caused by gram-negative rod-shaped bacteria known as Bacillus anthracis. Which are toxin-producing, encapsulated, facultative anaerobic organisms
The bacteria are typically found in soil, where they naturally reside. Domesticated ruminants and wild animals ingest spores from the soil.
The bacteria produce extremely potent toxins responsible for flu-like symptoms.
Anthrax is an infection that can spread from animals to humans, known as a zoonotic disease.
Symptoms, once noticed and if not treated promptly, can lead to pneumonia, septicemia, shock and eventually, death.
Transmission of Anthrax
Anthrax is an infection that can spread from animals to humans, known as a zoonotic disease.
Humans who come directly in contact with infected animals or their products, like waste, meat, milk and hide, can be exposed to spores through inhalation or ingestion.
In humans, infection is usually [but rarely] acquired through contact with the skin of an infected individual with skin lesions.
Inhalational infections are uncommon, while infections in the oropharynx, meninges, and gastrointestinal tract are rare.
“The potential use of Anthrax as a biological weapon has increased fear of this pathogen. Spores have been prepared in very finely powdered form (weaponized) to be used as agents of warfare and bioterrorism; in anthrax bioattacks of 2001, spores were spread in envelopes delivered via the United States Postal Service.”
(Bush & Vazquez-Pertejo, 2023b)
Pathophysiology of Anthrax
The spores of Bacillus anthracis can remain in the soil, wool, or animal hide for decades. The dry environment isn’t favourable for its growth, so it doesn’t grow while still there.
Once it enters a favourable environment, like tissue or blood [rich in amino acids and glucose], the spores germinate and multiply.
Human infection can be acquired by
- Cutaneous contact (most common)
- Ingestion
- Inhalation
- Injection
Cutaneous Anthrax
People can get infected when they contact animals, animal products [meat, hide, milk], or soil containing spores.
An open wound or abrasion increases susceptibility; however, an infection can still occur when the skin is intact.
Usually, cutaneous Anthrax is not contagious. However, in extremely rare cases, it can be spread from one person to another through direct contact or contact with contaminated objects.
Gastrointestinal (including oropharyngeal) Anthrax
Inadequately cooked meat [hide (‘ponmo’), bush meat, smoked meat] containing the vegetative forms of the anthrax organism can lead to infection when there is a break in the pharyngeal or intestinal mucosa.
If Anthrax is ingested, it can cause lesions ranging from the oral cavity to the cecum.
The toxin released by the infection can cause hemorrhagic necrotic ulcers and mesenteric lymphadenitis, ultimately resulting in intestinal haemorrhage, obstruction, or perforation.
Pulmonary Anthrax (inhalation anthrax),
Caused by breathing in spores and can be lethal. It typically results from exposure to contaminated animal products in the workplace, such as hides [ponmo].
“Gastrointestinal anthrax and inhalation anthrax are not transmitted from person to person.”
Once the spores enter the body, they will germinate inside macrophages. These macrophages then move to the regional lymph nodes, where the bacteria multiply. However, in inhalation anthrax, the spores will be deposited in alveolar spaces, which will be ingested by macrophages that will then move to mediastinal lymph nodes resulting in hemorrhagic mediastinitis.
“The predominant toxins are edema toxin and lethal toxin. A cell-binding protein, called protective antigen (PA), binds to target cells and facilitates cellular entry of edema toxin and lethal toxin. Edema toxin causes massive local edema. Lethal toxin triggers a massive release of cytokines from macrophages, which is responsible for the sudden death common among people with anthrax infection.”
(Bush & Vazquez-Pertejo, 2023b)
Symptoms and Signs of Anthrax

Patients with Anthrax typically exhibit symptoms within 1 to 6 days after exposure. However, in cases of inhalation anthrax, the incubation period can extend beyond six weeks.
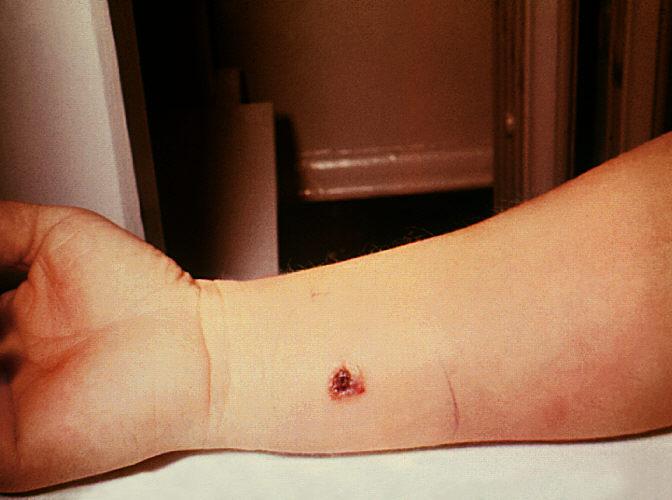
Cutaneous Anthrax
After exposure to infective spores, a painless and itchy red-brown bump appears within 1 to 10 days.
The bump grows and is surrounded by a red and swollen area. It also becomes filled with fluid and hardens; a central ulcer forms, followed by a black scab known as the malignant pustule.
It’s common to experience local swelling of lymph nodes, as well as malaise [weakness], myalgia [muscle aches], headache, fever, nausea, and vomiting.
Healing of the wound and resolution of swelling may take several weeks.
Gastrointestinal Anthrax
Ranges from having no symptoms to being life-threatening.
Common symptoms include fever, nausea, vomiting, abdominal pain, and bloody diarrhoea.
Ascites, a buildup of fluid in the abdomen, may also occur.
In severe cases, the intestines may die [intestinal necrosis], leading to a dangerous bloodstream infection [septicemia].
Oropharyngeal Anthrax
Manifests as swollen areas with ulcers and tissue death on the tonsils, back of the throat, or roof of the mouth.
The neck may also become swollen, and lymph nodes in the neck may enlarge.
Symptoms include voice changes, painful throat, fever, and difficulty swallowing.
The airway can become blocked.
Inhalation Anthrax
The symptoms of inhalational Anthrax start similar to the flu [common cold] and gradually worsen.
Within a few days, the fever worsens, and chest pain and respiratory distress become severe.; this is followed by cyanosis, shock, and coma.
Additionally, severe hemorrhagic necrotizing lymphadenitis develops and spreads to adjacent mediastinal structures.
Other symptoms include serosanguineous transudation, pulmonary oedema, and bloody pleural effusion.
In rare cases, Anthrax can also lead to hemorrhagic meningoencephalitis or gastrointestinal issues.
Management, Treatment and Diagnosis of Anthrax

It’s crucial to consider a person’s work and environmental exposure history.
These investigations are the primary [laboratory] methods of diagnosing Anthrax:
- Gram stain and culture
- Direct fluorescent antibody (DFA) test and polymerase chain reaction (PCR) assay
When testing for Anthrax, it’s crucial to examine samples from various identified sites like skin or mucous membrane lesions, blood, pleural fluid, cerebrospinal fluid, ascites, or stool.
It’s important to understand that Sputum examination and Gram stain may not be effective in detecting inhalation anthrax as there is often no airspace disease present.
However, a PCR test and immunohistochemical methods like DFA can assist in diagnosis.
Using nasal swab testing to detect spores in individuals who may have been exposed to inhalation anthrax is not advisable; this is due to the uncertainty surrounding the accuracy of a negative result. A negative test result does not guarantee that the person has not been exposed to anthrax spores. On the other hand, a positive result may indicate exposure.
A chest X-ray or CT scan can be done if respiratory symptoms are present. It reveals swollen hemorrhagic lymph nodes and pleural effusion. Pneumonic infiltrates are uncommon.
If a patient shows signs of meningitis or experiences a change in their mental state, it is recommended to perform a lumbar puncture.
If this is not feasible, central nervous system imaging through CT or MRI with contrast should be conducted to document the characteristics of meningeal enhancement for meningitis and identify hemorrhagic parenchymal lesions for anthrax meningoencephalitis.
While an enzyme-linked immunosorbent assay (ELISA) can detect antibodies in serum, confirming with a 4-fold increase in antibody titer from acute to convalescent specimens is necessary.
Anthrax is not contagious, which means you can’t catch it like the cold or flu.
Treatment
Anthrax is caused by bacteria and can be treated effectively with antibiotics. Additionally, treating flu-like symptoms, muscle aches, and dehydration can be very helpful in managing the illness.
- Antibiotics
- Other medications [supportive therapy]
- Pleural fluid drainage
Delaying treatment for Anthrax, often due to missed diagnosis, can increase the risk of death.
Cutaneous Anthrax
If there’s no significant swelling, general symptoms, or inhalational exposure, treatment is effective with one of the following antibiotics for 7 to 10 days.
- Ciprofloxacin
- Levofloxacin
- Moxifloxacin
- Doxycycline
Inhalation and other forms of Anthrax
In treating cutaneous Anthrax with significant swelling or symptoms, it is necessary to treat them with three antibiotics.
The antibiotic treatment should consist of at least two antibiotics that can kill bacteria, and one of them should be a protein synthesis inhibitor that can prevent the production of toxins.
Penicillin G is considered equally effective as fluoroquinolone if the B. anthracis strain is susceptible to penicillin.
Treatment should be given intravenously for ≥ 2 weeks or until the patient is clinically stable, whichever is longer.
After completing IV combination therapy, it is important to continue treatment with a single oral antibiotic for 60 days to prevent the possibility of relapse due to ungerminated spores in the lungs.
Antibiotics that are suitable and effective for killing bacteria are called bactericidal antibiotics:
- Fluoroquinolone
- Carbapenem
- Vancomycin
- Penicillin-susceptible strains
Some antibiotics that are suitable for stopping protein synthesis are:
- Linezolid
- Clindamycin
- Rifampin
- Chloramphenicol
Other medications
While corticosteroids may be effective for meningitis and severe mediastinal oedema, there is insufficient evidence to evaluate their effectiveness fully.
In the case of inhalation anthrax, monoclonal antibodies like Raxibacumab and Obiltoxaximab can be used alongside antibiotics to target the protective antigen component of B. anthracis toxin.
These antibodies have shown success in animal models, particularly when administered early.
Additionally, IV anthrax human immune globulin, derived from vaccinated donors, can also be used with antibiotics to treat inhalation anthrax.
Prognosis
Inhalation anthrax can be treated with early diagnosis and intensive support, including mechanical ventilation, fluids, and vasopressors, which can help reduce its mortality rate.
- Inhalation and meningeal anthrax: 100%
- Cutaneous Anthrax: 10 to 20%
- Gastrointestinal Anthrax: About 40%
- Oropharyngeal Anthrax: 12 to 50%
Prevention of Anthrax
An anthrax vaccine is available for people at high risk of anthrax exposure, such as military personnel, veterinarians, laboratory technicians, healthcare professionals and textile mills processing importing goat hair.
This vaccine is made of a cell-free culture filtrate containing protective antigen protein and no live or dead bacteria.
There is also a separate vaccine available for veterinary use.
To ensure protection, individuals must receive a 5-dose intramuscular vaccine series before exposure.
The primary series and booster vaccinations are about 93% effective. However, local reactions can occur from the vaccine.
Postexposure prophylaxis
Postexposure measures include
- Antibiotics
- Vaccination
- Monoclonal antibodies
Asymptomatic people (including pregnant women and children) exposed to inhaled Anthrax require prophylaxis with one of the following oral antibiotics given for 60 days:
- Ciprofloxacin
- Doxycycline
- Levofloxacin
- Moxifloxacin
- Clindamycin
When ciprofloxacin and doxycycline are not recommended, amoxicillin taken three times daily can be considered as a treatment option for susceptible organisms to penicillin.
It has been found that spores are present in the lungs after being exposed to aerosol. This means that individuals who are exposed to these spores are at risk of inhalation anthrax as the spores remain in their lungs even after the initial exposure. In order to eliminate any germinating organisms, antibiotic therapy is provided for a period of 60 days.
According to the Centers for Disease Control and Prevention (CDC), individuals who have been exposed to anthrax spores should receive the anthrax vaccine along with antibiotic prophylaxis.
According to the CDC, the recommended vaccine schedule involves three doses given subcutaneously at 0, 2, and 4 weeks accompanied by antimicrobial therapy for at least 60 days.
Raxibacumab and obiltoxaximab are monoclonal antibodies indicated for prophylaxis of inhalation anthrax when alternative therapies are not available or are not appropriate.
In Conclusion
Anthrax is an infection that can be properly treated if detected early. And in the case of an outbreak, it’s important to put measures in place to curtail its spread. People must be educated on how to prevent it from infecting them and how to detect infections and promptly seek medical expert help.
Further Studies
- Guide to Understanding Athrax | CDC
- Photos of Anthrax | CDC
- Anthrax | World Health Organisation
- Current State of Anthrax Vaccines and Key R&D Gaps Moving Forward | National Library of Medicine
- Anthrax Vaccine Research Program (AVRP) | CDC
References
- Anthrax. (n.d.). https://www.who.int/europe/news-room/questions-and-answers/item/anthrax
- Bush, L. M., & Vazquez-Pertejo, M. T. (2023, May 25). Anthrax. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/infectious-diseases/gram-positive-bacilli/anthrax
- Nigerian Government Raises Alarm Over Outbreak Of Anthrax In West Africa, Calls For Vaccinations | Sahara Reporters. (2023, June 12). https://saharareporters.com/2023/06/12/nigerian-government-raises-alarm-over-outbreak-anthrax-west-africa-calls-vaccinations
- Nwafor. (2023). Ponmo: What you should know about Anthrax. Vanguard News. https://www.vanguardngr.com/2023/06/ponmo-what-you-should-know-about-anthrax/
- What is Anthrax? | CDC. (n.d.). https://www.cdc.gov/anthrax/basics/index.html
Seen something that looks out of place or do you have a comment or suggestion? Reach out to the editors here: info@carecityonline.com.



Drop Your Comment